The Union’s landmark pharma reform moves from technical drafting to political bargaining. Negotiators are preparing for tense debates over how to reward innovation against antibiotic resistance and support treatments for rare diseases.
During the last pharma package trilogue in Strasbourg, negotiators focused on the inclusion of patients and healthcare professionals within the European Medicine Agency’s committees, their voting rights, and the work of scientific working parties, rapporteur Tiemo Wölken (S&D/DEU) told EU Perspectives.
“The work is moving steadily. As we are working on a long text, negotiations will take time,” he said. “The next rounds are likely to become “more political.”
The next trilogue, scheduled for 10–11 November, is expected to mark the transition from technical drafting to political negotiation. According to Mr Wölken, discussions should begin on the incentive framework for antimicrobial resistance (AMR) and orphan medicines. Though much will depend on progress at expert level.
You might be interested
“During the November trilogue we should start touching up on the more political topics such as the AMR incentives and potentially orphans. However, this will depend on the progress the technical level will make till then. It is too early to go into details,” he said.
During the November trilogue we should start touching up on the more political topics such as the AMR incentives and potentially orphans. — MEP Tiemo Wölken (S&D/DEU)
The rapporteur added that medicine shortages are also expected to become one of the most contentious areas as negotiations intensify. The Danish Presidency, which chairs the Council side, hopes to reach a political agreement before the end of its term.
Industry urges stronger AMR incentives
Industry groups warn that the current Transferable Exclusivity Voucher (TEV) design risks falling short. A recent report by the European Federation of Pharmaceutical Industries and Associations (EFPIA) argues that while both EU institutions have kept the scheme, “They have also introduced substantial modifications which risk weakening the effectiveness of the TEV.”
The Commission’s original design could deliver around €294m per voucher. But restrictions added by Parliament and Council, including tighter eligibility, a €490m revenue cap, and reduced duration, cut its estimated value to €162 million. This is less than half the intended incentive.
EFPIA says the TEV should be strengthened and paired with complementary mechanisms. Such as subscription or revenue-guarantee models to meet Europe’s €1.3bn per antibiotic “fair-share” contribution to global AMR incentives.
A deepening innovation gap
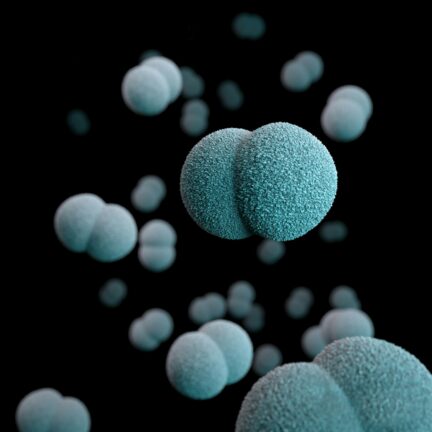
The debate comes after WHO released new reports exposing the fragile state of global antibiotic R&D and diagnostics. The 2025 Analysis of antibacterial agents in clinical and preclinical development shows the number of antibacterials in the clinical pipeline dropped from 97 in 2023 to 90 in 2025. Only 15 qualify as innovative, and five are effective against one of WHO’s “critical” priority pathogens.
“Antimicrobial resistance is escalating. But the pipeline of new treatments and diagnostics is insufficient,” said Dr Yukiko Nakatani, WHO Assistant Director-General for Health Systems. “Without more investment in R&D, together with dedicated efforts to ensure that new and existing products reach the people who most need them, drug-resistant infections will continue to spread.”
WHO urges coordinated investment across discovery, diagnostics and equitable access. This needs to be underpinned by novel funding models to sustain small and medium-sized innovators. This is a call that echoes Europe’s own trilogue debate.
Stronger global pull models
At the World Health Summit in Berlin on 14 October, the session “Push, Pull, Partner: Building a Global AMR Incentive Ecosystem” brought together policymakers, researchers, and non-profit leaders to discuss how to make antibacterial R&D both sustainable and equitable.
Adnaan Ghanchi, senior program director at ARMoR, described the scale of the market failure. “Developing new antibiotics is really really hard… failure rates are astronomical. You spend half a billion dollars to develop a drug and nobody wants it on the other end,” he said.
Developing new antibiotics is really really hard… failure rates are astronomical. You spend half a billion dollars to develop a drug and nobody wants it on the other end. — Adnaan Ghanchi, Senior Program Director at ARMoR
He pointed to the UK’s “Netflix-style” subscription model as the “poster child for pull funding”. He explained that under the scheme, “They guarantee the pharma companies that they will buy this drug for the next ten years regardless of how much they use.”
But Mr Ghanchi also warned that the EU’s current voucher proposals remain underpowered. “We probably need a billion euros per product,” he said. “And this voucher scheme is somewhere between €150m and €400m worth of incentive. “And that’s just for the EU’s fair share alone,” he stressed.
Rohit Malpani, Senior Adviser at the Global Antibiotic Research and Development Partnership (GARDP), agreed that simply copying traditional market logic will not work. “If we try to have pull incentives try to replicate the current pharmaceutical market, it’s not going to succeed,” he said. Instead, incentives should focus on small and medium-sized developers that “don’t otherwise have an exit strategy to bring new products to market”.
Mr Malpani stressed that funding mechanisms must blend push and pull tools while embedding equity as a core principle: “We are not going to get access to those antibiotics where they’re required, or develop new antibiotics for children and babies unless we have push funding for it, because it’s just not commercially interesting.”
Beyond AMR
While antimicrobial incentives dominate headlines, rare disease advocates have warned that the trilogue’s outcome could also reshape Europe’s orphan drug framework.
In its June 2025 position paper, EURORDIS, Rare Diseases Europe, urged negotiators to preserve ambition and clarity. The group backs a “simple, two-tier exclusivity system” maintaining the current ten-year baseline and adding “a higher reward for therapies meeting the high unmet medical need definition”.
Predictability, EURORDIS argues, “remains one of the few tools capable of attracting sustained investment in rare diseases”. It also calls for restoring explicit recognition of orphan medicinal products in the EMA’s PRIME scheme, warning that removing this reference “risks creating uncertainty for developers”.
On incentive modulation, EURORDIS urges deleting the vague criterion that medicines must show a “meaningful reduction in morbidity or mortality”, calling it “difficult to apply consistently”.
For EURORDIS, success in the trilogue will hinge on “clear rules, adequate incentives and meaningful patient involvement”. Getting that balance right, it concludes, “means offering real and justified hope to those still waiting for a treatment”.